The Science of
Patient Decisions
Why patients say "I need to think about it" and what you can do about it. This guide reveals the psychology behind treatment decisions and how visual communication changes everything.
See How It Works
BEFORE
Patient photo
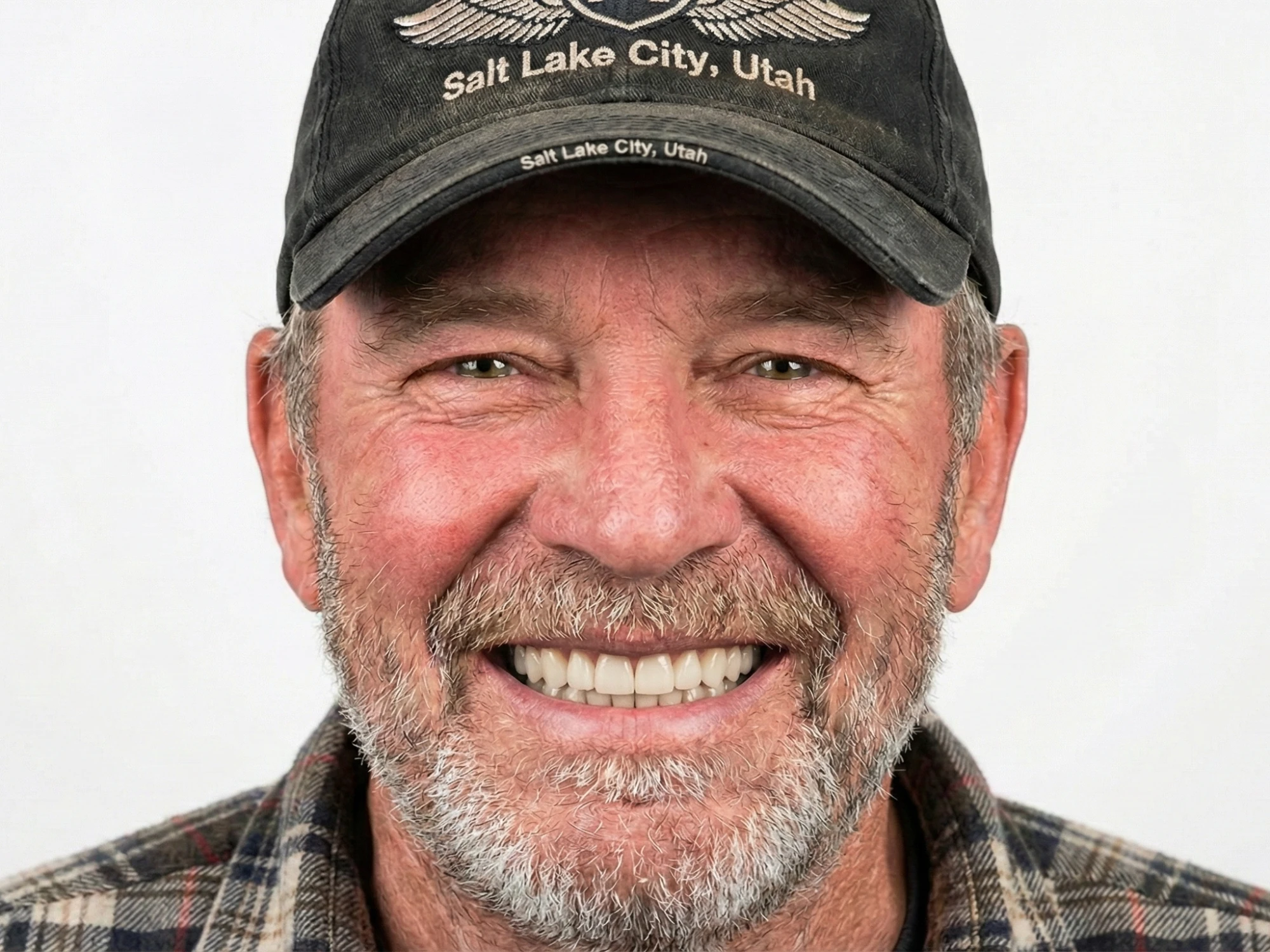
AFTER
Xadia simulation in 30 seconds
Would you say yes without seeing this?
Your Patients Aren't Saying "No"-They're Saying "I Can't See It"-And That's Costing You Cases Every Single Day.
You've experienced this scene dozens of times...
A patient sits across from you. They're clearly unhappy with their smile. They've taken time off work to come see you. They've been thinking about this for months, maybe years.
You explain the treatment plan. You describe how their smile will look. You use all your expertise to paint a picture with words...
And then they say it:
"I need to think about it."
They leave. And 70% of the time, they never come back.
But here's what most dentists don't realize:
That patient didn't reject your treatment plan. They rejected the uncertainty of not knowing what they'd get.
Think about it...
Would you pay $5,000, $10,000, or $20,000 for something you couldn't see? Would you commit to a major change based purely on someone's description?
Of course not.
Yet that's exactly what we ask patients to do every day.
The Psychology of Decision-Making
What research tells us about how patients actually decide...
Let's talk about what's actually happening in your patient's brain during a consultation.
Neuroscience research has shown that humans are visual creatures. We process images 60,000 times faster than text.1 And when it comes to making decisions, what we can see carries far more weight than what we're told.
The Visualization Effect
Studies show that when people can visualize an outcome:
- They're 3x more likely to take action2
- Their fear and anxiety decrease significantly7
- They make decisions faster and with more confidence2
- They're less likely to experience regret afterward2
Why "Seeing Is Believing" Is Literally True
When a patient sees a simulation of their potential smile, something powerful happens in their brain:
The same neural pathways that process actual experiences light up.
In other words, when they see themselves with a beautiful smile, their brain begins treating it as real.4 The emotional connection to that future outcome strengthens. The decision shifts from "Should I do this?" to "How do I get this?"
"The brain doesn't distinguish clearly between a vividly imagined future and an experienced memory. When patients see their simulated smile, they're not imagining-they're experiencing."4
This is why showing beats telling. Every single time.
Words vs. Visuals
Why even the best communicators are fighting an uphill battle...
You might be thinking: "I'm a great communicator. My patients trust me. I can explain things well."
And you're probably right.
But here's the problem:
Words create different pictures in different minds.3
When you say "beautiful, natural-looking smile," your patient might imagine something completely different from what you're picturing. Their reference points, past experiences, and expectations all filter your words through their own lens.
"We'll straighten your teeth and whiten them. Your smile will look more balanced and natural."
Patient thinks:
- • "What does 'balanced' mean?"
- • "How white is 'natural'?"
- • "Will I like it?"
- • "This is a big investment..."
"Here's what your smile could look like after treatment. What do you think?"
Patient thinks:
- • "That's actually me!"
- • "I love how that looks!"
- • "I need to show my family..."
- • "When can we start?"
The difference isn't subtle. It's dramatic.
One conversation ends with uncertainty. The other ends with excitement and action.

BEFORE
The patient's starting point

AFTER
Their personalized simulation
No amount of words can replace what this image communicates instantly.
The Family Factor
Why decisions don't happen in your office...
Here's something that might surprise you:
Most cosmetic dental decisions aren't made in your consultation room.6
They're made at the dinner table.
They're made when your patient goes home and their spouse asks, "So what did the dentist say?"
And this is where most practices lose cases without ever knowing it.
Your patient loved the idea in your office. But when they got home, they couldn't explain it. They couldn't show their partner what they'd look like. And without that shared vision, the enthusiasm faded.
The Consultation Continues at Home
Think about major purchase decisions in your own life. Whether it's a car, a house renovation, or any significant investment...
You discuss it with your family. You want their input. Their support.
Your patients are no different.
A spouse who can't visualize the outcome becomes a barrier. Not intentionally-they simply can't support what they can't see.
But when your patient can share a simulation link...
When their partner can see exactly what they'll look like...
That barrier becomes a bridge.
The Sharing Advantage
When patients can share their simulation with family:
- Family members become advocates for treatment
- Decisions happen faster with shared buy-in
- Patients feel more confident with support
- "Let me think about it" becomes "Let me show my partner"
Traditional Approaches & Their Limitations
Understanding why common methods fall short...
Before we talk about solutions, let's be honest about what practices have been doing-and why it hasn't been working.
Approach #1: Stock Before/After Photos
You've probably used these. Generic photos of other patients' transformations.
The problem? They're not your patient.
When patients see someone else's results, their brain immediately flags it: "That's not me. I might not look like that."
The emotional connection is minimal. The trust transfer is weak.
Approach #2: Manual Photo Editing
Some practices use Photoshop or similar tools to manually edit patient photos.
This can work, but it comes with serious drawbacks:
- Time-intensive: 15-30 minutes per simulation
- Skill-dependent: Results vary by operator
- Inconsistent: Quality differs from day to day
- Expensive: Staff time costs add up quickly
- Not scalable: Can't do this for every patient
Approach #3: Verbal Descriptions Only
This is still the most common approach. Relying purely on words to paint the picture.
We've already discussed why this is the least effective method. Words create ambiguity. Ambiguity creates hesitation. Hesitation becomes "I'll think about it."
There had to be a better way...
The Modern Approach
How technology is changing patient consultations...
What if you could show every patient exactly what their smile could look like...
In 30 seconds?
Without any design skills?
With consistent, professional results every time?
This is what modern smile simulation technology makes possible.

BEFORE
Upload a patient photo

AFTER
Get a realistic preview in seconds
What Good Simulation Technology Does
- Creates personalized previews using the patient's actual photo
- Delivers results instantly during the consultation
- Requires no special skills from your team
- Produces consistent quality every single time
- Enables easy sharing so patients can discuss at home
- Maintains professional appearance with your clinic branding
The Impact on Case Acceptance
When practices implement effective smile simulation:
These aren't magic numbers. They're the natural result of addressing the fundamental barrier to patient decisions: uncertainty.
Best Practices for Implementation
How to get the most from smile simulation technology...
Having the technology is one thing. Using it effectively is another.
Here's what we've learned from practices that see the best results:
Practice #1: Show Early, Not Late
Don't wait until the end of the consultation to show the simulation. Use it early to capture attention and frame the entire conversation.
When patients see their potential smile first, they listen to the treatment details with enthusiasm rather than skepticism.
Practice #2: Make It Collaborative
"Let's take a look at what's possible together."
Frame the simulation as exploration, not sales. You're helping them discover possibilities. This removes pressure and builds trust.
Practice #3: Always Offer Sharing
Before they leave, ask: "Would you like me to send you a link so you can show your family?"
This accomplishes two things:
- It respects their need to discuss with loved ones
- It ensures the conversation continues at home-with visuals
Practice #4: Use It for Remote Consultations
Patients can capture their own photos from home and send them to you. You create the simulation and share it back. The entire consultation can happen virtually.
This opens up possibilities for patients who can't easily visit in person-and for practices looking to expand their reach.
Practice #5: Train Your Entire Team
Everyone who interacts with patients should understand the technology and be able to use it. Consistency across your team creates a seamless patient experience.
Ready to Transform Your Consultations?
See how smile simulations can help your patients say yes to treatment.
Addressing Common Concerns
What practice owners often ask...
"Won't patients expect their results to look exactly like the simulation?"
This is the most common concern-and it's valid. The key is framing. Simulations are presented as possibilities, not promises. Use language like "This gives you an idea of what we can achieve" rather than "This is exactly what you'll look like." Proper disclaimers and honest communication actually build more trust, not less.
"My staff doesn't have time for another tool."
Good simulation technology should save time, not add to it. When consultations are more effective, you spend less time on follow-ups, re-explanations, and patients who never convert. A 30-second simulation often replaces 15 minutes of verbal explanation.
"We've done fine without it so far."
The question isn't whether you can succeed without it-you probably already have. The question is: how much better could your case acceptance be? How many patients said "I'll think about it" and never came back? Patient expectations are rising. They're used to visualizing outcomes in every other industry.
"Is the technology accurate enough?"
Modern simulation technology has become remarkably sophisticated. It's not about creating a photo-perfect prediction-it's about giving patients a realistic sense of the transformation. When done well, simulations provide enough accuracy to build confidence without creating false expectations.
Key Takeaways

BEFORE
Before simulation

AFTER
After simulation
This is what transforms
- Patients don't reject treatment-they reject uncertainty
- Visual communication is processed 60,000x faster than text
- Decisions often happen at home, not in your office
- Shareable simulations turn family members into advocates
- Modern technology makes professional simulations accessible to every practice
- Effective use of simulations can increase case acceptance by 35% or more
The science is clear. The technology exists. The only question is: are you ready to transform how your patients experience consultations?
Ready to Help More Patients
Say "Yes" to Treatment?
See how Xadia can transform your consultations with realistic smile simulations in seconds.
Sources & References
* Industry statistics and conversion data referenced in this guide are based on aggregated research and may vary by practice. Individual results depend on implementation, patient demographics, and practice-specific factors.